 New Treatment Option Proves Effective in Treating Prostate Cancer
New Treatment Option Proves Effective in Treating Prostate Cancer
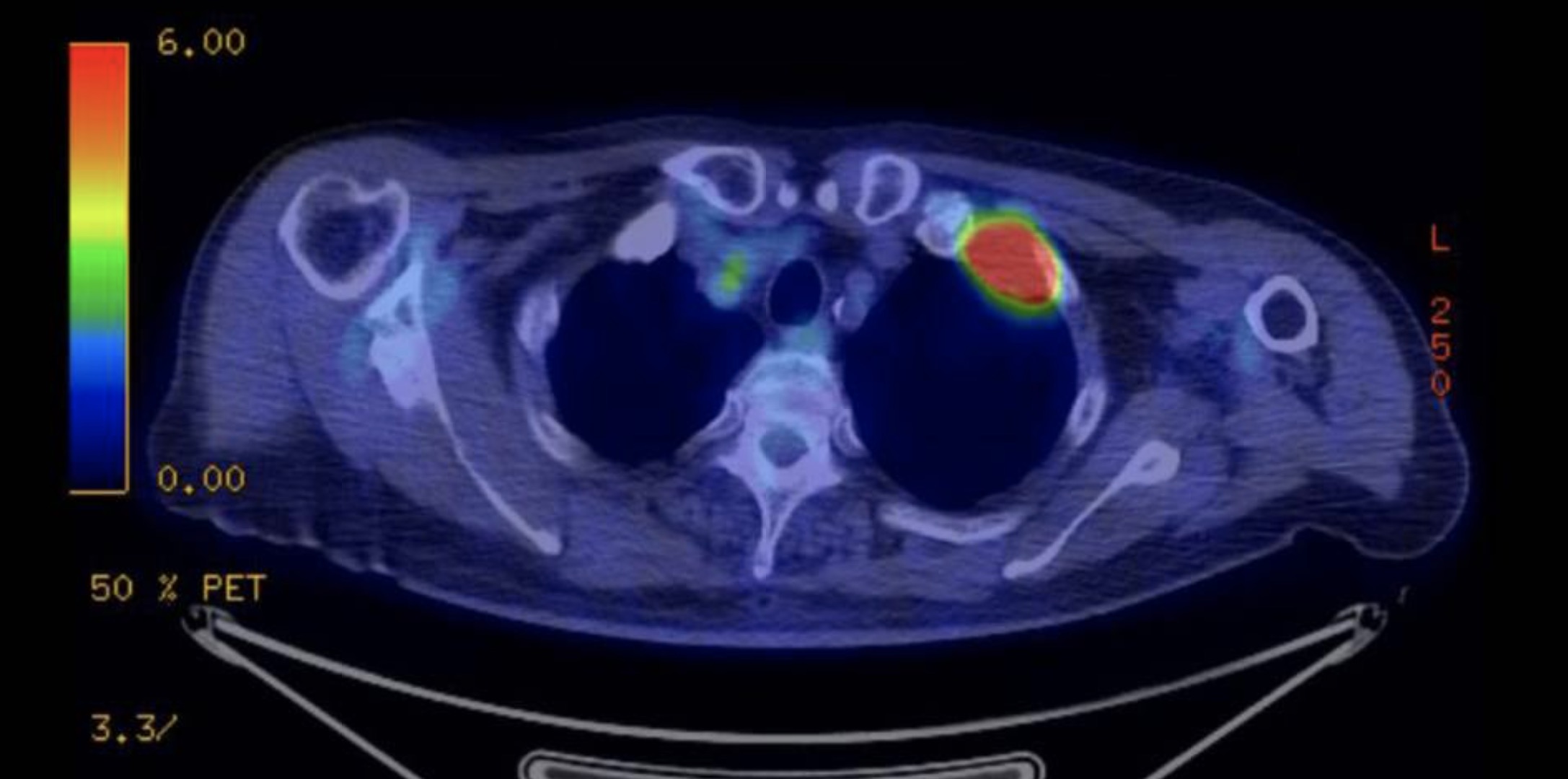
Prostate cancer is a prevalent disease that affects one in eight men in their lifetime. Traditionally, radiation or surgery have been the go-to treatment options. However, these methods come with significant side effects that can greatly impact a patient’s quality of life. Fortunately, new research presented at Salt Lake City’s Society of Interventional Radiology Annual Scientific Meeting has unveiled a promising alternative treatment option for prostate cancer – MRI-guided transurethral ultrasound ablation (TULSA).
TULSA represents a revolution in whole-gland prostate cancer treatment, according to Steven S. Raman, M.D., FASR, FSIR, a professor of radiology, urology, and surgery at UCLA. This innovative procedure involves inserting a catheter-like device through the urethra into the prostate. With the guidance of MRI, ten therapeutic ultrasound elements are precisely positioned inside the prostate. As the device rotates around the gland, MR thermometry monitors the tissue temperature, ensuring that it is heated to over 55 degrees Celsius without affecting the sensitive nerves surrounding it.
The key advantage of TULSA is its ability to maximize cancer cell destruction while minimizing collateral damage to the prostate. Dr. Raman explains that this procedure achieves the ultimate trifecta in prostate cancer treatment – complete local cancer control, potency, and continence in the urine. The precision offered by image-guided therapy significantly reduces complications commonly associated with traditional treatment options.
In a prospective observational study involving 115 men from 13 sites in five countries, TULSA demonstrated impressive results. One year after the procedure, 76% of patients had undetectable cancer on follow-up biopsy. Additionally, the median prostate volume decreased by 92%, and prostate-specific antigen (PSA) levels dropped from 6.3 ng/ml to 0.63 ng/ml. This reduction in PSA levels indicates a significant decrease in cancer markers and suggests successful treatment.
Furthermore, TULSA proved to have a very favorable side-effect profile compared to alternative surgical, radiation, and thermal therapies. Patients retained continence and erectile function even after five years of treatment, distinguishing TULSA as a promising option for long-term quality of life improvement.
Although TULSA showed great potential, the study also highlighted areas for improvement. Calcifications between the urethra and the target prostate cancer were identified as early predictors of TULSA failure. This discovery led to improved detection and management of prostate swelling and misalignment during the procedure, reducing preventable errors and ensuring better treatment outcomes.
Dr. Raman emphasizes that interventional radiologists are well-suited to detect and manage prostate cancer, just as they handle lung, kidney, and liver cancers. Their expertise in image-guided procedures and ablation makes them an important component of prostate cancer treatment.
While further research is necessary to validate the findings of the study, TULSA has the potential to change the standard of care for thousands of men with prostate cancer. With its minimally invasive approach and impressive results, TULSA offers hope for improved outcomes and quality of life for patients battling this disease.
In conclusion, the development of MRI-guided transurethral ultrasound ablation represents a significant advancement in prostate cancer treatment. By minimizing side effects while maximizing cancer control, TULSA offers a durable alternative to traditional treatment options. As further research is conducted, the medical community eagerly anticipates the potential impact that TULSA could have on prostate cancer care worldwide.