 The Link Between Diabetes Medications and Gastric Paralysis
The Link Between Diabetes Medications and Gastric Paralysis
A recent investigation has discovered a concerning correlation between two popular medications, Ozempic and Wegovy, used for diabetes management and weight reduction, and an increased risk of developing gastric paralysis. Gastric paralysis, also known as gastroparesis, affects the muscles of the stomach and can cause food to remain in the organ for extended periods of time.
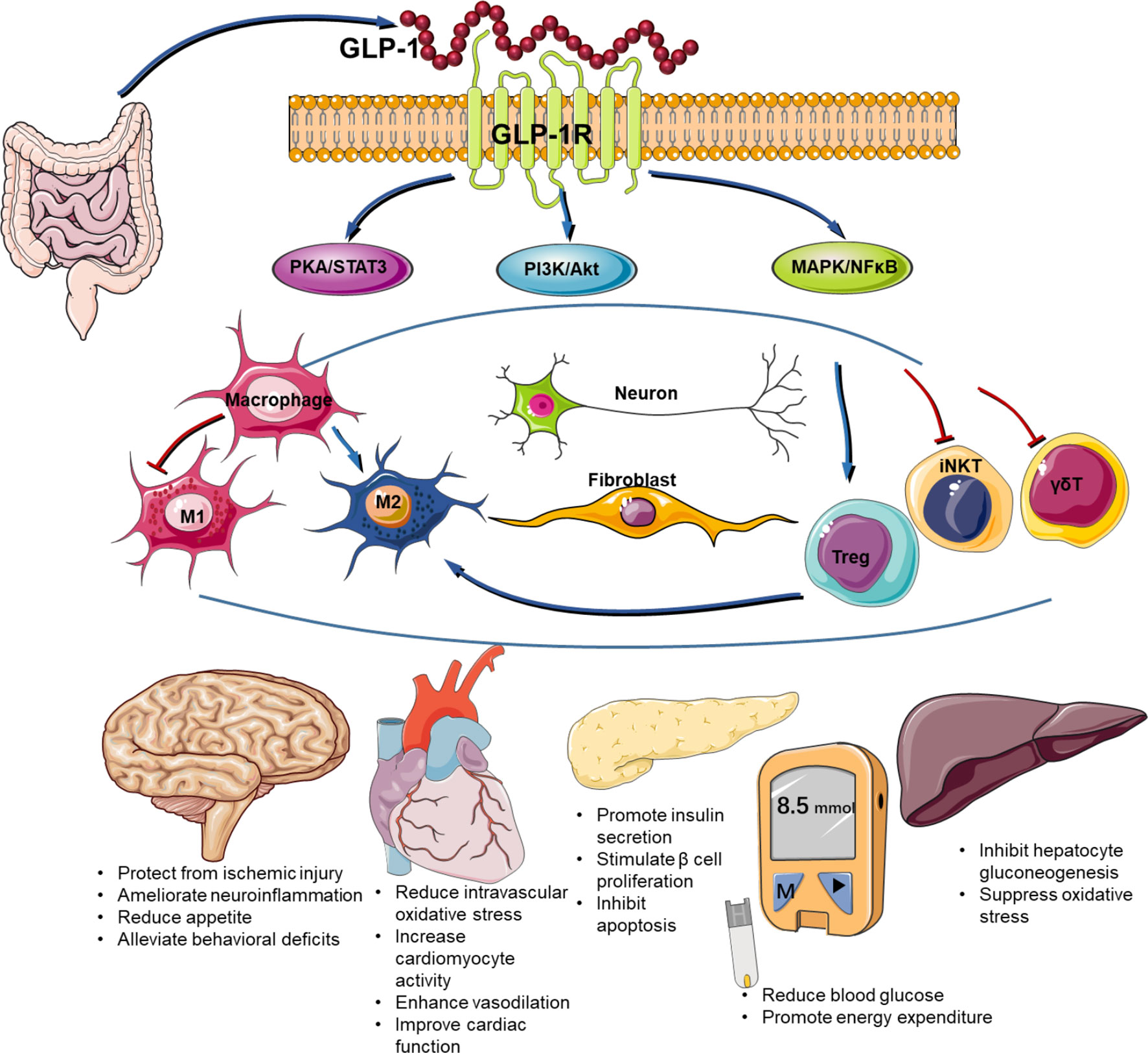
Wegovy has been approved by the US Food and Drug Administration (FDA) for weight management purposes, while Ozempic is primarily used to help individuals with type 2 diabetes manage their blood sugar levels. However, Ozempic is occasionally prescribed for weight loss, despite lacking FDA approval for this purpose. Both medications are injectables that contain semaglutide, a protein similar to the hormone glucagon-like peptide-1 (GLP-1), which plays a crucial role in promoting insulin synthesis after eating.
In addition to the well-known gastrointestinal side effects such as nausea, vomiting, and diarrhea, recent research has uncovered less common side effects of these medications. GLP-1 receptor agonists or GLP-1 analogues, such as Ozempic and Wegovy, have been found to potentially cause acute pancreatitis, ileus, and gastric paralysis (gastroparesis). These findings were presented at the Digestive Disease Week 2024 conference.
The study conducted by researchers from the University of Kansas involved analyzing data from 185,000 obese or diabetic patients who were prescribed GLP-1 analogs between December 2021 and November 2022. The researchers discovered that the likelihood of developing gastroparesis had increased by 66%, affecting approximately 0.53% of the patients. Cholecystitis, or gallbladder inflammation, was observed in 0.55% of the patients and was predicted to be 28% more likely to develop in the future.
Another alarming finding was that 0.04% of patients who took GLP-1 analogs experienced drug-induced pancreatitis, with the probability of developing this condition increasing by over 350%. Furthermore, 7.5% of patients had a higher incidence of gastroesophageal reflux disease (GERD), where stomach contents travel up the esophagus, and 9% experienced a significant increase in nausea and vomiting.
The study’s authors concluded that the use of GLP-1 agonists in patients with diabetes and obesity is associated with various gastrointestinal side effects, including nausea, vomiting, gastroparesis, GERD, esophagitis, drug-induced pancreatitis, cholecystitis, and the need for upper-endoscopy.
A separate trial assessed the risk of gastroparesis in patients with type 2 diabetes who were taking GLP-1 receptor agonists. The study involved over 336,000 patients, with one cohort receiving the drug and the other not. The researchers found that gastroparesis was more prevalent in patients taking GLP-1 receptor agonists at 6, 9, 12, 18, and 24 months. The odds of developing gastroparesis increased significantly after six to twenty-four months of treatment.
In another study conducted by researchers at the Mayo Clinic in Minnesota, the impact of GLP-1 receptor agonists on gastrointestinal symptoms was assessed. Data from approximately 80,000 individuals who received prescriptions for these medications were analyzed. The findings revealed that around 18% of patients experienced at least one new gastrointestinal symptom indicative of gastroparesis. Approximately one-third of this group underwent gastric emptying scintigraphy (GES), a test that evaluates the stomach’s ability to empty.
Based on the study’s abstract, the researchers concluded that these real-world data suggest a high prevalence of gastrointestinal symptoms in individuals treated with GLP-1 receptor agonists.
In light of these studies, it is essential for healthcare providers and patients to be aware of the potential risks associated with Ozempic, Wegovy, and other GLP-1 analogs. While these medications offer benefits for diabetes management and weight reduction, it is crucial to monitor patients for any signs of gastrointestinal complications and make informed decisions regarding their use.